Learn More About
Periodontal (Gum) Disease
Brussels, 3 February 2021. COVID-19 patients are at least three times more likely to experience complications if they also have gum disease, according to research published in the Journal of Clinical Periodontology,1 the official publication of the European Federation of Periodontology (EFP).
The study of more than 500 patients with COVID-19 found that those with gum disease were 3.5 times more likely to be admitted to intensive care, 4.5 times more likely to need a ventilator, and almost nine times more likely to die compared to those without gum disease.
Blood markers indicating inflammation in the body were significantly higher in COVID-19 patients who had gum disease compared to those who did not, suggesting that inflammation may explain the raised complication rates.
“The results of the study suggest that the inflammation in the oral cavity may open the door to the coronavirus becoming more violent,” said Professor Lior Shapira, EFP president-elect. “Oral care should be part of the health recommendations to reduce the risk for severe COVID-19 outcomes.”
Periodontitis, a serious form of gum disease, affects up to half of all adults worldwide.2 Periodontitis causes inflammation of the gums and, if left untreated, inflammation can spread throughout the body. COVID-19 is associated with an inflammatory response that may be fatal. This study investigated the relationship between periodontitis and COVID-19 complications.
This was a nationwide case-control study conducted in Qatar, which has electronic health records containing medical and dental data. The study included 568 patients diagnosed with COVID-19 between February and July 2020. Of these, 40 had complications (intensive care unit [ICU] admission, ventilator requirement, or death) and 528 did not. Information was collected on gum disease and other factors that might be associated with COVID-19 complications including body mass index (BMI), smoking, asthma, heart disease, diabetes, and high blood pressure. Data were also obtained on blood levels of chemicals related to inflammation in the body.
Of 568 COVID-19 patients in the study, 258 (45%) had gum disease. After adjusting for age, sex, BMI, smoking status, and other conditions, the odds ratios for COVID-19 complications in patients with gum disease, compared to those without gum disease, were 3.67 (95% confidence interval [CI] 1.46–9.27) for all COVID-19 complications, 3.54 (95% CI 1.39–9.05) for ICU admission, 4.57 (95% CI 1.19–17.4) for ventilator requirement, and 8.81 (95% CI 1.00–77.7) for death.
The authors stated: “If a causal link is established between periodontitis and increased rates of adverse outcomes in COVID-19 patients, then establishing and maintaining periodontal health may become an important part of the care of these patients.”
Professor Mariano Sanz of the Complutense University of Madrid, Spain, one of the study’s authors, noted that oral bacteria in patients with periodontitis can be inhaled and infect the lungs, particularly in those using a ventilator. He said: “This may contribute to the deterioration of patients with COVID-19 and raise the risk of death. Hospital staff should identify COVID-19 patients with periodontitis and use oral antiseptics to reduce transmission of bacteria.”
Professor Shapira said that the association between periodontitis and lung diseases including asthma, pneumonia, and chronic obstructive pulmonary disease (COPD) is well established.3 He said: “This study adds further evidence to the links between oral health and respiratory conditions. Periodontitis is a common disease but can be prevented and treated.”
Professor Nicola West, EFP secretary general, added: “This study highlights another association between gum disease and our systemic health and reiterates the need for ongoing, lifelong dental care for people susceptible to gum disease and a strong preventive approach to periodontitis for populations as a whole.”
What you can do to prevent gum disease
- Brush your teeth carefully more than once a day using a manual or powered toothbrush.
- Clean between your teeth daily using an interdental brush (or floss if the gaps are too tight).
- Specific mouth rinses or toothpastes can be used on top of cleaning to reduce inflammation.
- Do not smoke, maintain a healthy weight, eat a balanced diet, exercise, reduce stress.
- If you have diabetes, control your blood sugar.
The scientific paper ‘Association between periodontitis and severity of COVID‐19 infection: a case‐control study’ is publicly available at https://onlinelibrary.wiley.com/doi/10.1111/jcpe.13435![]()
The European Federation of Periodontology (EFP) is a non-profit organisation dedicated to promoting awareness of periodontal science and the importance of gum health. Its guiding vision is “Periodontal health for a better life.”
Founded in 1991, the EFP is a federation of 37 national periodontal societies that represents more than 16,000 periodontists, dentists, researchers and oral-health professionals from Europe and around the world. It pursues evidence-based science in periodontal and oral health, promoting events and campaigns aimed at both professionals and the public.
The EFP organises EuroPerio, the world’s leading congress in periodontology and implant dentistry, as well as other important professional and expert events such as Perio Master Clinic and Perio Workshop. The annual Gum Health Day, on 12 May, organised by the EFP and its member societies, brings key messages on gum health to millions of people across the world.
The EFP also organises workshops and outreach campaigns with its partners: projects have covered the relationship between periodontal disease and diabetes, cardiovascular disease, and caries, as well as women’s oral health during pregnancy.
The EFP’s Journal of Clinical Periodontology is the most authoritative scientific publication in this field and the federation also publishes a monthly digest of research (JCP Digest) and the quarterly Perio Insight magazine which offers expert views and debates.
The federation’s work in education is also highly significant, notably its accredited programme for postgraduate education in periodontology and implant dentistry.
The EFP has no professional or commercial agenda.
Funding: This study received no funding.
Disclosures: The authors declare no conflict of interest relevant to this study.
References
1) Marouf N, Cai W, Said KN, et al. Association between periodontitis and severity of COVID-19 infection: a case-control study. J Clin Periodontol. 2021. doi:10.1111/jcpe.13435. The article was first published as an accepted article on 1 February 2021. This article has been accepted for publication and undergone full peer review but has not been through the copyediting, typesetting, pagination, and proofreading process, which may lead to differences between this version and the version of record.
2) Nazir MA. Prevalence of periodontal disease, its association with systemic diseases and prevention. Int J Health Sci. 2017;11:72–80.
3) Gomes-Filho IS, da Cruz SS, Trindade SC, et al. Periodontitis and respiratory diseases: A systematic review with meta-analysis. Oral Dis. 2020;26:439–446.
Brushing your teeth regularly and maintaining proper oral care can play a big role in the fight against COVID-19 — since patients with gum disease are nine times more likely to die from the bug, according to new research.
A study of more than 500 patients also found that those with gum disease were 3.5 times more likely to be admitted to intensive care and 4.5 times more likely to need a ventilator, Medical Xpress reported.
In addition, coronavirus patients with poor gum health are at least three times more likely to experience complications, according to the study published in the Journal of Clinical Periodontology.
Blood markers indicating inflammation in the body were markedly higher in patients with gum disease, suggesting that inflammation may explain the raised complication rates.
“The results of the study suggest that the inflammation in the oral cavity may open the door to the coronavirus becoming more violent,” said study co-author Professor Lior Shapira of the Hebrew University in Israel.
“Oral care should be part of the health recommendations to reduce the risk for severe COVID-19 outcomes,” added Shapira, president-elect of the European Federation of Periodontology.
Periodontitis, a serious form of gum disease that affects up to half of all adults worldwide, can spread throughout the body if left untreated — and COVID-19 is associated with an inflammatory response that may be fatal.
The study, which was conducted in Qatar, included 568 patients diagnosed with COVID-19 between February and July 2020.
Of those, 40 had complications — including admission to the ICU, being placed on a ventilator, or death — and 528 did not.
Other factors including body mass index, asthma, heart disease, diabetes, blood pressure and smoking also were taken into account in COVID-19 complications. Data also were obtained on blood levels of chemicals related to inflammation in the body.
The chances of death for COVID-19 patients with gum disease was 8.81 times higher than others, while the chances of ending up in intensive care or on a ventilator were 3.54 and 4.57 times greater, respectively.
“If a causal link is established between periodontitis and increased rates of adverse outcomes in COVID-19 patients, then establishing and maintaining periodontal health may become an important part of the care of these patients,” the authors wrote.
Professor Mariano Sanz of the Complutense University of Madrid, Spain, one of the authors, said that oral bacteria in patients with periodontitis can be inhaled and infect the lungs.
“This may contribute to the deterioration of patients with COVID-19 and raise the risk of death. Hospital staff should identify COVID-19 patients with periodontitis and use oral antiseptics to reduce transmission of bacteria,” he said.
Shapira said the link between periodontitis and lung diseases including asthma, pneumonia and chronic obstructive pulmonary disease is well established.
Originally published on FoxNews![]()
While you may think that some loss of teeth is inevitable as we age, it is actually possible for all of your teeth to last a lifetime. One of the ways you can achieve this goal is to avoid periodontal disease (“peri” – around; “odont” – tooth), which is caused by bacteria that attack the tissues around the teeth. Unfortunately, you may not even realize you have gum disease as the signs and symptoms are not always as apparent to you as they are to a dental professional.
Nearly all people who do not maintain good daily oral hygiene will develop gingivitis. If left untreated, this bacterial gum infection can progress from gingivitis (“gingival” – gum; “itis” – inflammation) to periodontitis, which results in bone loss around your teeth. As the bone tissue is lost, the gum tissues detach from the teeth and form little pockets that provide an even better place for bacteria to live — where your brush and floss can’t reach. As periodontal disease advances leading to more bone loss, tooth loss can result. Part of this has to do with genetics, as periodontal disease tends to run in families. The good news is that periodontal disease can be controlled, even at more advanced stages.
Signs and Symptoms of Periodontal Disease
It’s important to understand that you can have periodontal disease with no obvious symptoms, especially if you are a smoker (nicotine reduces blood supply preventing bleeding and swelling of the gum tissues). Still, there are some important things to look for:
- Bleeding gums — Some people think that when their gums bleed, it simply means they’re brushing too hard. While brushing too hard is bad for the gums, it should not cause bleeding. Any bleeding of the gums should be considered a warning sign of gum disease.
- Bad breath — It’s very easy for plaque to collect in the spaces between the teeth, creating the perfect living conditions for bacteria that produce odorous, sulfur-containing compounds, resulting in bad breath.
- Redness or swelling of the gums — Inflammation of the gums is usually the first visible sign of periodontal disease.
- Receding gums — If you notice that your teeth look longer than they used to, it may be that your gum tissue has receded (away from the enamel), exposing some of your tooth roots.
- Sensitivity — If there is gum recession, the exposed roots may become sensitive to hot or cold.
- Periodontal abscess — Bacteria can become enclosed in a periodontal pocket and the area will fill with pus, becoming swollen and painful.
- Loose teeth — When periodontal disease results in bone loss, teeth can become loose or migrate. Tooth loss can result and may be accelerated if you are applying excessive biting forces from clenching or grinding your teeth.
Periodontal Disease & Your Overall Health
 Periodontal disease starts in your mouth but has actually been linked to more serious conditions, such as cardio-vascular disease (CVD), diabetes and preterm births. Research has suggested two plausible mechanisms for how gum disease and these other serious medical concerns could be related: moderate to severe periodontal disease increases the level of systemic (bodily) inflammation — a characteristic of all chronic inflammatory diseases. Also, the same bacterial strains that are commonly found in periodontal pockets surrounding diseased teeth have been found in blood vessel plaques of individuals with CVD. Therefore, it may be helpful to reduce periodontal inflammation to reduce systemic inflammation.
Periodontal disease starts in your mouth but has actually been linked to more serious conditions, such as cardio-vascular disease (CVD), diabetes and preterm births. Research has suggested two plausible mechanisms for how gum disease and these other serious medical concerns could be related: moderate to severe periodontal disease increases the level of systemic (bodily) inflammation — a characteristic of all chronic inflammatory diseases. Also, the same bacterial strains that are commonly found in periodontal pockets surrounding diseased teeth have been found in blood vessel plaques of individuals with CVD. Therefore, it may be helpful to reduce periodontal inflammation to reduce systemic inflammation.
Treatment Options
All periodontal therapy starts with the evaluation of your oral hygiene techniques and instruction for improving them, followed by the mechanical removal of plaque and any calcified deposits (tartar or calculus) that are present on the root surfaces. This is accomplished with a cleaning technique known as scaling, root planing or debridement using hand instruments and/or ultrasonic (high frequency vibrational) instruments. Locally applied antimicrobial products or antibiotics might also be recommended during various parts of periodontal treatment to assist in healing and pocket-depth reduction, hopefully eliminating the need for periodontal surgery. Sometimes surgical procedures may be necessary to remove the deep pockets that form between inflamed gum tissue and teeth. There are many different types of surgery to handle a variety of problems. And many times, combinations of procedures are used to attempt to reduce the number of surgeries as well as the cost of treatment.
Can brushing and flossing actually save your life? Researchers are asking that question as they learn more about the link between periodontal (gum) disease and heart disease.
Periodontal disease is caused by poor oral hygiene. By brushing your teeth twice a day and flossing once a day, you remove plaque, a sticky film of bacteria that forms on teeth. If you skip flossing or brushing, then the bacteria will irritate and inflame the gums, causing the gum tissue to pull away from the teeth and create pockets. More bacteria settle into these pockets, and if left untreated, can destroy the bone and tissue holding the teeth in place. Periodontal disease is the leading cause of tooth loss in Americans over the age of 35.
Now it’s been linked to heart disease, too. The bacterial byproducts from gum disease enter the bloodstream and trigger the liver to make a certain kind of protein that can inflame the arteries and cause blood clots that could clog the arteries, leading to heart attack and stroke, according to a study published in the Journal of Periodontology![]() .
.
“The mouth is the gateway to the entire body,” explained Dr. Charles Laun, a dentist at Coast Dental South Lakeland. “Everything that’s in your mouth, from the food you eat to the bacteria that forms, winds up in your body.”
Researchers have found that people with gum disease are almost twice as likely to suffer from coronary artery disease as people without gum disease, according to the American Academy of Periodontology![]() . Periodontal disease can also worsen existing heart conditions, researchers report. Patients who have had a cardiac procedure within the previous year and patients at risk of endocarditis, which is an infection of the inner lining of the heart, may require an antibiotic prior to dental procedures that cut the gum and allow bacteria to enter the bloodstream.
. Periodontal disease can also worsen existing heart conditions, researchers report. Patients who have had a cardiac procedure within the previous year and patients at risk of endocarditis, which is an infection of the inner lining of the heart, may require an antibiotic prior to dental procedures that cut the gum and allow bacteria to enter the bloodstream.
How do you know if you have gum disease?
“The best thing patients can do is make sure the dentist takes measurements around their teeth,” Dr. Laun advised. “Many patients tell me they have never had their gums probed before. I tell them, you need to know what’s happening under the gum line as well as above. It’s like looking at the walls of your house. You can paint them and make them look pretty, but if you have termites, then the walls are eventually going to fall down – and the damage is going to be much more extensive and expensive to fix. If you have bacteria attacking the bone and tissue holding your teeth in place, then the problem needs to be treated and eliminated.”
In addition to saving your teeth, you could be helping your heart. Now that’s a reason to love your dentist!
It’s a goal we all have: We want to walk into the dentist’s office, hear that our teeth look great, get a routine cleaning, and then not have to think about going to the dentist again for another six months.
It can come as a shock when that doesn’t happen. You might think you’re taking great care of your teeth: You brush twice a day, you floss somewhat regularly, and occasionally use a mouthwash. So how can a dentist diagnose you with periodontal disease?
Your Lifestyle Affects Your Smile
Often, it’s the choices you make every day that can lead to periodontal disease. You may have begun to skip brushing in the morning because you were in a rush to get out the door, or at night because you were so tired. You may be using a toothbrush that is more than three months old and its bristles are not as effective. You may not be flossing every day, so bacteria (plaque) builds up between your teeth and under your gum line, attaching to the root surface. After only 48 hours, the plaque can calcify and will be there until you have your teeth cleaned again, said Dr. Michael Quinn, a periodontist with more than 20 years of experience who practices at several Coast Dental offices in Georgia.
Small changes in our hygiene habits can add up to big problems for your mouth very quickly. At Coast Dental, the dentist uses x-rays and an oral examination to determine how healthy your teeth and gums are, following the classification system established by the American Academy of Periodontology (AAP). Over time, untreated gum disease causes the gum to separate from the teeth, forming a bacteria-filled pocket that becomes infected. Our clinicians use a tiny ruler called a probe to measure the depth of the gum tissue around each tooth, known as a sulcus, to see if a pocket has formed. As the disease progresses, the pockets become deeper and the treatments become more extensive, more expensive and more time-consuming. Periodontal disease is the number one cause of adult tooth loss in the United States; ignoring it could allow the disease to deteriorate the bone and gums so badly, teeth will need to be extracted.
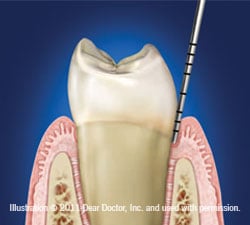 Healthy Mouth
Healthy Mouth
Here is an illustration of a healthy mouth. Clinical findings include 0-3 mm sulcus, no bone loss, pink and firm gums, no bleeding on probing and no root exposure. A doctor or hygienist typically can perform a routine cleaning.
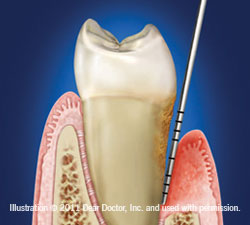
 Slight Chronic Periodontitis
Slight Chronic Periodontitis
Clinical findings include 4-6 mm pockets, and could include bleeding on probing, pus present, plaque and calculus present, slight root exposure, bone loss and slight clinical attachment loss. The patient’s treatment plan typically requires Scaling and Root planing and adjunctive medications / laser treatments and may require the patient to return more frequently for treatment.
 Advanced Periodontitis (Irreversible) Clinical findings include 6 mm or greater pockets, red, swollen gums, and could include bleeding on probing, pus present, plaque and calculus present, severe root exposure, bone loss, severe clinical attachment loss and loose teeth. The patient’s treatment plan typically requires Scaling and Root planing and adjunctive medications / laser treatments and may require the patient to return more frequently for treatment. The general dentist may also refer the patient to a periodontist for treatment due to the advanced nature of bone loss.
Advanced Periodontitis (Irreversible) Clinical findings include 6 mm or greater pockets, red, swollen gums, and could include bleeding on probing, pus present, plaque and calculus present, severe root exposure, bone loss, severe clinical attachment loss and loose teeth. The patient’s treatment plan typically requires Scaling and Root planing and adjunctive medications / laser treatments and may require the patient to return more frequently for treatment. The general dentist may also refer the patient to a periodontist for treatment due to the advanced nature of bone loss.
A woman just diagnosed with Chronic Periodontitis was not thinking of her own health as she sat in the dental office. Instead, she wanted to know if her children were at risk too.
It’s a common question, said Dr. Michael Quinn, a Periodontist with 14 years of experience who practices at several Coast Dental locations in Atlanta, Georgia. “The short answer is no. Gum disease is not like the common cold. You cannot transmit gum disease to your children through kissing or using the same silverware,” Dr. Quinn explained. “It’s true that bacteria in mom’s mouth can be transmitted to the child’s mouth. But the bacteria that cause chronic periodontitis need to be in just the right spot in just the right amount in just the right ecological niche to cause harm. This just doesn’t happen.”
The children’s immune response to fight infection and their inflammatory response are different than in adults, and do not allow the gum disease-causing bacteria to take hold.
Chronic periodontitis is an infection of the gums caused by the build-up of plaque, a sticky material made of bacteria and food debris that accumulates on the tooth. If the plaque is not removed by brushing and flossing daily, then it hardens into a substance called tartar. Tartar pushes the bacteria deeper into the gum tissue, which irritates and inflames the gums. The bacteria cause the gums to become infected and swollen and to pull away from the tooth, creating pockets where more bacteria will accumulate. If the infection is allowed to fester, the disease destroys the gum tissue and bones, and your teeth could become loose and eventually fall out or need to be extracted.
In the rare occasions when children do have periodontitis, it is usually Aggressive Periodontitis, which can be associated with a systemic disease like Diabetes, Leukemia or Down Syndrome, Dr. Quinn said. In a survey of 263 Type I diabetics, 11 to 18 years of age, 10 percent had overt periodontitis, according to the American Academy of Periodontology. Children with Down Syndrome may have teeth that are not well-aligned, creating more areas where bacteria may be trapped and lead to infection. It’s important these kids follow their dentist’s advice, using the types of toothbrushes, toothpaste and floss recommended for their particular condition. Often, their pediatric dentist will recommend they see a periodontist for further evaluation and treatment.
Even though most children aren’t susceptible to the most devastating kinds of gum disease, kids do suffer from Chronic Gingivitis. Chronic Gingivitis is the first stage of gum disease, and the only stage that is reversible. Symptoms may include red or puffy gums which may bleed when brushed. If your child sees blood in the sink or on the toothbrush, the child needs to see a dentist.
“I cringe when I see a mom point a finger at a kid and say, ‘I told you that you should be brushing,'” Dr. Quinn said. “Good habits start with the parents checking the kids’ oral hygiene habits, watching them brush their teeth and checking their gums to make sure they’re not red or swollen. Parents should be brushing and flossing their children’s teeth until the kids are old enough to do it themselves. Most children will still need supervision until they are comfortable doing it correctly by themselves.”
While Chronic Gingivitis is often a sign of poor oral hygiene, tweens and teenagers can have hormonal gingivitis. Girls are most susceptible to gingivitis when they are menstruating. Older teenagers, age 16 through 19, start to be susceptible to more advanced forms of periodontitis. It can be exacerbated if the teenagers are not brushing or flossing, or if there is family history of gum disease.
“If one of my patients has no medical conditions but does have Aggressive Periodontitis, I tell them to tell everybody in their family – brothers, sisters, parents, aunts, uncles and children,” Dr. Quinn said. “They need to know there is a family history, and their family members need to tell their dentists so they can be extra vigilant during exams. Since Aggressive Periodontitis runs in families, it’s very important the children’s dentist knows to look for it.”
The good news is most children won’t have to worry about periodontitis when they’re young, and if they brush their teeth correctly and floss daily, they may be able to avoid getting gum disease forever.